Learning to accept my limitations has increased my freedom!
At the first sight of a slight tremor in my left pinky finger, I was fascinated. I would often show people like it was something funny! Sort of like tricks that you could do when you were a kid (ie. touching your tongue to your nose) and saying, ‘Look what I can do!”
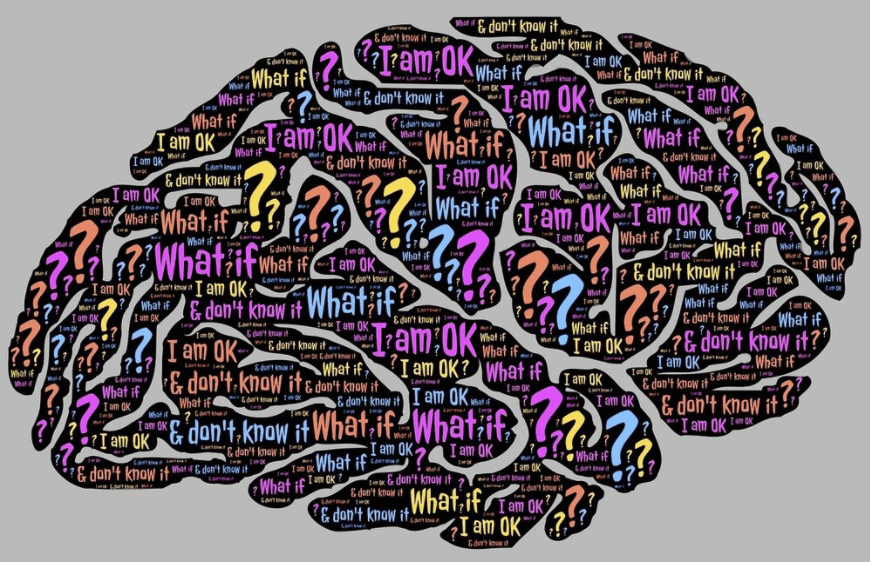
When that tremor slowly spread its way through my fingers and up my arm, it quickly became something that I tried desperately to hide. If I was making a presentation, I would hold that arm behind my back. If I was in a meeting, I would sit on that hand to cover it up. I would often clasp my hands together and dig my thumb into the palm of my left hand to try to gain some control as though causing pain would trick my brain into sending a different response. Trying to hide the tremor became harder. And it seemed the more I was aware of it, the harder it was to control.
For those of you without a tremor, it can be hard to understand. But if you’ve ever participated in a sport that required you to hold a position (ie. weight lifting, yoga, rock-climbing etc.) then you might have experienced a tremor-like feeling. When rock climbing, we called it ‘sewing machine leg’ – your leg would shake involuntarily when you were trying to reach for your next hold.
Recently I started doing Spin classes (group cycling classes on stationary bicycles). This is a great workout for me as it is high intensity, with no risk of falling off the bike! During my last class, we were climbing up a steady hill and working hard. The instructor shouted out at us to ‘embrace the shake’ in our leg muscles as the climb got slower and more difficult.
I smiled.
Great advice.
Trying to hide something that can’t be hidden is useless.
Embrace the shake.