“Nobody told me there’d be days like these. Strange days indeed.” – John Lennon
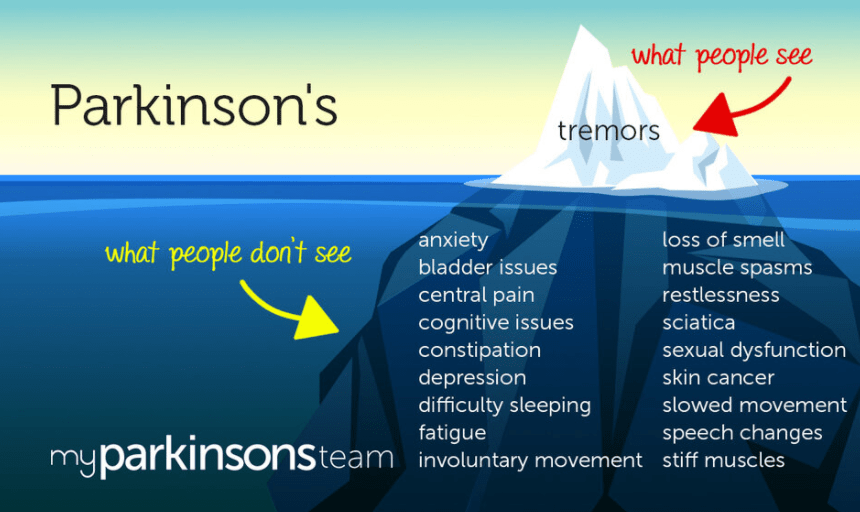
I’ve been thinking about whether or not to write this post for a couple of weeks now. You see, I’ve fallen into a pattern of writing about a PD symptom or issue, and either providing my own solution, a recommended remedy, or simply trying to put a positive spin on living with this chronic neurological degenerative disease.
Truth is though, I’ve fallen into a bit of a rough patch lately. And I’ve decided to write about it in order to let readers know my truth, my pain, and just how much I dislike having Parkinson’s. Today I will not be strong, or brave, or light, or even positive. I’ll be me.
I’ve written that Exercise is Medicine and how moving fast allows me to feel free. Well three weeks ago I injured my ankle. My right ankle. My good ankle. The ankle I rely upon to maintain good balance. There was no grand event to cause the injury, just overuse from walking/running. Tendon? Ligament? Bone? Nobody is completely sure, but rest is what I need for it to heal.
More appointments are made; Physio. Osteo. Xray. Bone Scan in a couple of weeks. Because I have Osteoporosis, we need to figure out what’s going on with my bones. This scares me silly. Are my bones becoming so weakened that walking fast/running is too risky?
I am benched. Sidelined. Totally knocked off my game.
If I don’t move, I get stiff. I get rigid. Stuck. My muscles contract constantly – even during sleep. Pain is multiplied and wide spread. Shoulder, neck, back, butt, knees, calves, feet.
I wake up each morning feeling as though I’ve gone 10 rounds and lost.
I don’t like the feeling of losing. I’m not very good at it.
Yesterday, I walked around my block (maybe 400m). It’s a start. (ok…there it is…a little hint of positivity! I can’t help it!)